| visit: www.infertilitytutorials.com |
|
A normal menstrual cycle requires a precisely timed series of events that interrelate to allow for regular ovulation.
These events are important to understand since they allow physicians to manage fertility care.
(Available Drawing: Hypothalamus-Pituitary-Ovarian Axis)
(1) Development of a monthly pool of recruitable follicles No recruited follicle will enter more than one cycle of maturation, such that if a follicle begins to mature with FSH stimulation the follicle will either ovulate or will degenerate during that month.
Clinical importance The goal of menotropin therapy generally is to mature as many eggs as possible. Since only that month’s recruited follicles can respond to FSH and develop you are not using eggs that would ever enter another cycle. Therefore, you will not have early menopause due to menotropin therapy. (Available Drawing: Developmental Timecourse)
(2) FSH concentration increases a few days prior to the onset of menstrual flow
It is uncommon for 2 eggs to mature simultaneously in a cycle, with the twinning rate for natural cycles in the USA about 1 in 80 to 1 in 90 pregnancies. Circulating FSH concentration decreases as ovulation approaches to enhance atresia (degeneration) of the maturing nondominant follicles
Clinical importance
(3) The growth rate and hormonal function of the dominant follicle changes during the cycle
Clinical importance
(4) Circulating luteinizing hormone (LH) concentration increases dramatically about 36 hours
(one and a half days) prior to ovulation
Clinical importance
Detection of the LH surge (as LH excreted in urine) is the basis of the commercially available ovulation predictor
kits (purchased in the pharmacy).
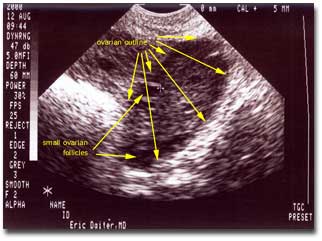
Available Photos:
(5) The follicular cyst rapidly changes following ovulation under the influence of
increased LH to become a "corpus luteum" cyst. Granulosa cells are cells that line the inside of both of these cysts and are capable of producing either estrogen or progesterone. Cholesterol is the starting material for either of these hormones and its molecular structure is changed using proteins called enzymes. The activity of the enzymes that change cholesterol into either estrogen or progesterone can be enhanced or suppressed within these granulosa cells. Under conditions present prior to ovulation the granulosa cells produce mostly estrogen and under the conditions present following ovulation these cells produce mostly progesterone. Prior to ovulation, high circulating estrogen concentrations act on the endometrium (uterine lining) to stimulate growth that results in an increased endometrial thickness. Following ovulation, the high circulating concentration of progesterone acts on the endometrium to stabilize it and prepare it for the implantation of an embryo.
Clinical importance Supplemental progesterone for a luteal phase deficiency is usually continued until about 10-12 weeks gestation (8-10 weeks from fertilization). The placenta takes over progesterone production from the ovarian corpus luteum during this time, so that further supplementation is not necessary.
(6) The "window of uterine receptivity" is a short period of time during which embryos may
implant into the uterus Progesterone is believed to be the major determinant of the window of receptivity, however, many other candidate hormones and protein messengers are also being considered as the research on molecular mechanisms of implantation continues to grow The duration of the window of uterine receptivity in humans is thought to be about 3 days
Clinical importance If progesterone production, or the uterine response to the progesterone produced, is not adequate then the lining of the uterus may be inadequate for embryo implantation. This situation can lead to either infertility if the lining does not become receptive or recurrent pregnancy loss if the lining is receptive for implantation but the embryo cannot develop normally.
(7) Menses occur if a pregnancy is not achieved In a pregnancy cycle, the maternal circulation begins to have a detectable hCG concentration about 7 to 8 days after fertilization (fertilization occurs within a day or so of ovulation). This hCG then takes over (by acting like LH) the stimulation of progesterone production by the corpus luteum cyst. If the woman does not become pregnant, then there is no hCG to take over the role of LH in the support of the corpus luteum cyst. Thus, the corpus luteum cyst deteriorates, the progesterone concentration supporting the uterine lining declines and the uterine lining that has grown in preparation for pregnancy is shed (as the menstrual flow).
Clinical importance | |||||||||||||||||